- Dermal Fillers
- Hyaluronidase
Hyaluronidase - The Ultimate Guide
Hyaluronidase injection and administration procedure is described by Mona, an aesthetic nurse, who emphasizes the significance of comprehending its use in aesthetics.
Introduction:
The aesthetics sector is growing and is expected to be worth over $5 billion in 2023. Non-surgical procedures already account for 75% of the market. In the US, a lot of training days are organized to prepare participants to buy and use hyaluronic acid HA filler for their patients' anti-aging needs. However, as we all are aware, the skill of administering injections is only one component of this treatment; other aspects involve knowledge and understanding of anatomy and physiology, consenting concerns, aftercare, and, most significantly, complication management. On support forums, networking groups, and study days, I notice that practitioners regularly bring up the subject of how to address complications. The fact that so many medical professionals lack the confidence and expertise to handle the negative emotions that may be so devastating to a patient is a troubling sight. The purpose of this page is to provide the reader with important information on the usage of hyaluronidase, including how it functions and—most importantly—when to administer it.
Known as dispersants, hyaluronidases are a class of injectable enzymes. These aid in accelerating the hydrolysis process that breaks down hyaluronic acid naturally. It is frequently used "off license" in aesthetics despite being approved for therapeutic uses such as enhancing tissue permeability to improve medication administration or accelerate the absorption of subcutaneous fluids. Off-label usage refers to the prescription and administration of a drug in a manner that differs from that which is permitted but does not necessarily imply that it is harmful to use. The license is received from the Healthcare Regulatory Agencies and will specify the age range of patients who may be treated with the medicine, how much to administer, and what it can be used for. Hyaluronidase can be administered in the event of an adverse reaction as long as the doctor is operating in the patient's best interests, their autonomy is respected, and the patient has given their complete permission. In order to decide how much hyaluronidase to use and how to reconstitute it because of this "off license" usage of hyaluronidase, practitioners must only consult with other specialists (along with their own knowledge), which can be constricting if one has limited experience utilising Hyaluronidase. The administration and dose will depend on a number of variables, including the concentration of HA filler, degree of cross-linking, and volume of HA deposit.
Hydase, Hylenex, Amphadase and Vitrase are currently the most popular brands on the US market, and that’s due to the fact that these specific brands received FDA approval. This also justifies why they are very costly (I’d say over priced). There are many other hyaluronidase brands out there that may be less popular yet do the exact same or even better job.
HA filler complications to be aware of
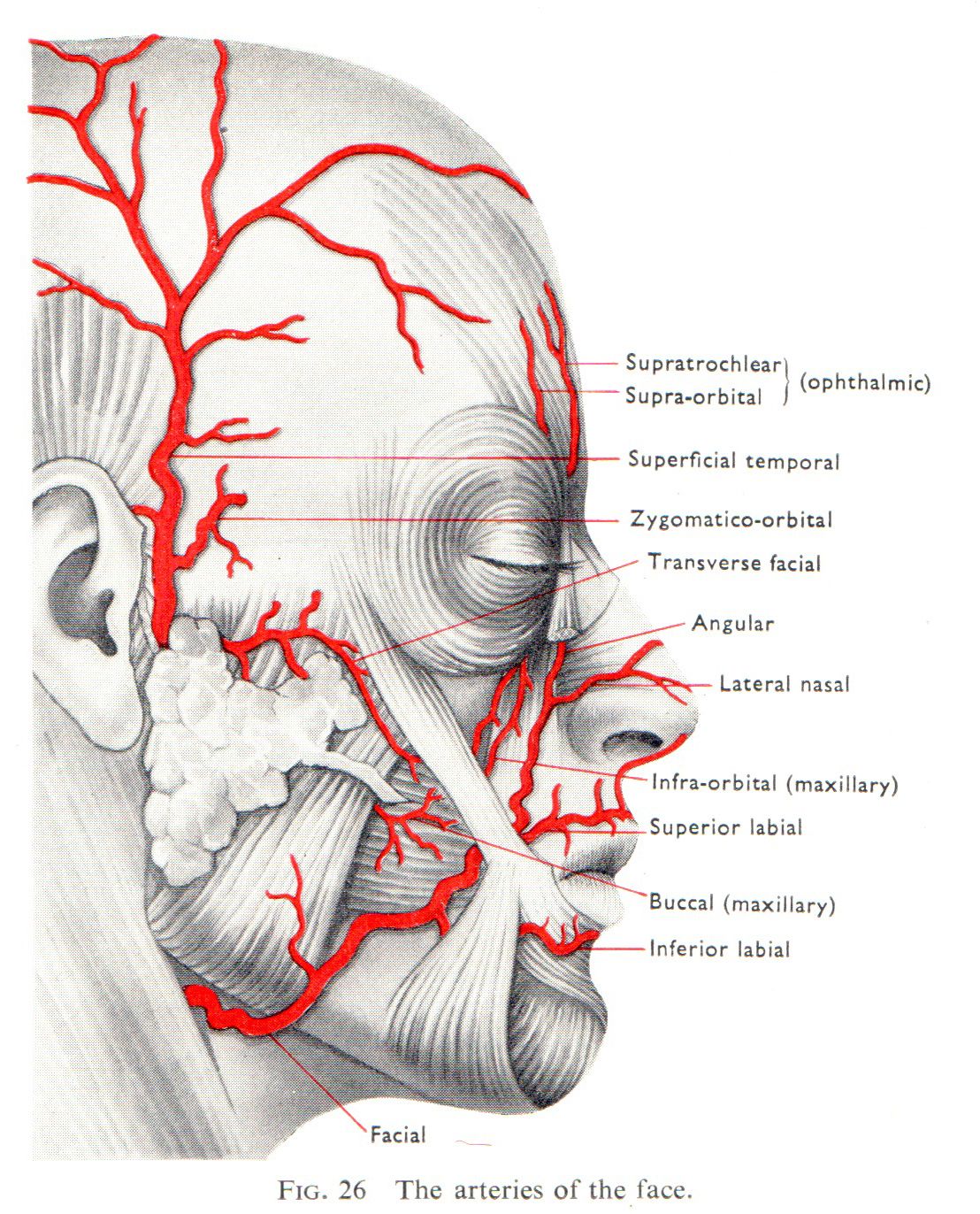
Of course, there are a number of risks involved with using a hyaluronic acid filler, including bruising, slight swelling, and discomfort where the injection was made. However, these side effects are easily handled by the patient with close monitoring and care. The more severe side effects, including those that occur when filler is injected into an artery or vein, will necessitate medical attention and the treatment with hyaluronidase injection. When a hyaluronic acid filler is injected into an artery, it may result in the filler itself blocking the artery or a clot forming surrounding the filler. Necrosis, an irreversible consequence that results in the loss of the skin tissue, can occur if the vessel plays a substantial role in providing blood to the skin. When the area of the skin does not receive enough blood and oxygen, this happens. A blockage brought on by hyaluronic acid filler into a vein can also result in blood moving backwards into the tissues, raising pressure and resulting in low grade ischaemia.

"Photo-Credit: Cassidy Valentine" - Necrosis in the lips
One of the most dreaded areas for necrosis after HA treatments is the nose, especially at the tip. Injecting dermal filler into the angular arteries surrounding the nose might potentially result in obstruction, skin necrosis, or, in exceedingly rare circumstances, blindness, illustrating how serious a vascular problem can be. Dermal Filler can migrate proximally to the internal carotid system after being injected into a facial artery, thereafter, upon pressure release, the substance enters the central retinal artery and may cause blindness or vision loss. In order to reduce the risk of adverse reaction, it is crucial that practitioners are able to spot the warning indications of an oncoming necrosis and possess the necessary abilities to respond immediately. In addition to having a policy in place that enables the practitioner to handle the situation, they also need to be completely competent and confident in their ability to handle it.
When should you use hyaluronidase?
When using HA dermal fillers, over-injection can be a danger that can leave the patient with undesirable lumps or looking "puffy," with huge volumes of filler visible in the mid-face. Anywhere on the face, nodules can develop after the dermal filler procedure. Those that appear within 48 hours of the injection may be inflammatory, but the ones that appear few weeks after the filler has been administered (or later) are more likely to include infection. (such fillers include but not limited to Juvéderm Ultra and Restylane).
Hyaluronidase can also be used to treat large haematomas. The use of hyaluronidase can enhance absorption via hypodermoclysis, which is the act of infusing fluids into the body through the interstitial or subcutaneous regions. It is critical to emphasise that if the practitioner detects infection, hyaluronidase should not be used and antibiotics should be recommended instead. The Tyndall effect, on the other hand, is a side effect that may be treated using hyaluronidase. This occurs when the HA is applied too superficially, resulting in a blue colouring of the skin.
The practitioner must keep an eye out for any indications of blanching of the skin, a change in look that may seem dark or mottled, during the treatment session. In this case, the patient may complain of discomfort, and the affected area may start feeling cold. If these warning signals are disregarded, the region may become blue, resulting in tissue necrosis. Hyaluronidase should be given as soon as this problem appears, and there is a good chance that tissue necrosis can be averted or made less severe if given early. Hyaluronidase should be utilised as soon as possible because its efficiency in decomposing HA fillers diminishes after around four hours. Whether the circumstance is an urgency or not, it is critical that the patient completely understands the consequences of why it is being given, how it will be delivered, and that a permission document be completed. Patients must also be informed of the potential risks that come with the usage of hyaluronidase.
Ovine Hyaluronidase vs Bovine hyaluronidase
There are several different origins of hyaluronidases, some are synthetic, some are human derived and there are also the Bovine and Ovine hyaluronidase which are in fact the most commonly used forms. Ovine hyaluronidase (ovine testicular hyaluronidase) has been shown in numerous tests to be more effective than Bovine hyaluronidase. They are both very effective and safe to use, however Ovine hyaluronidase (OTH) has occasionally been found to have superior qualities.
How to use hyaluronidase?
A common hyaluronidase v ial comes with 1500 IU of hyaluronidase in a powder for solution form to be reconstituted with saline NaCl. In this case here, we are covering hyaluronidase activity in cosmetic dermatology, where a filler injection is dissolved.
Hyaluronidase normally comes as a white-colored powder in a glass vial. Some come in liquid form. Hyaluronidase 1500 IU can be reconstituted as follows:
- 10 ml of 0.9% Saline should be drawn into a syringe.
- Introduce 1ml of saline-0.9% into the Hyaluronidase vial.
- To make sure the Hyaluronidase powder is fully dissolved, rotate the vials several times.
- With the remaining 9ml of saline in your syringe, draw up the 1ml of hyaluronidase mixture back into the syringe to create a concentration of 150-IU per ml. Hyaluronidase should be injected into the target region using a 27 gauge needle for the deeply placed fillers. Administration needs to be precise and restricted to the target area being treated. Occlusions should be treated with serial puncture injections of hyaluronidase down the course of the artery. It’s beneficial to massage the treated region during and after the Hyaluronidase treatment to maximize the outcome and promote mechanical breakdown. A reminder that Hyaluronidase only breaks down hyaluronic acid based fillers such as Restylane and juvéderm ultra, Belotero, or similar). Radiesse filler for example can't be dissolved with hyaluronidase since it is not a hyaluronic acid based dermal filler. Similarly for Sculptra which is also not composed of hyaluronic acid gel.
Local Anesthetic:
Some injectors utilise anesthetic products (topical or local anesthetic) or other related products that numb the area before the treatment to minimise discomfort. Using anesthetic products is totally fine and will not affect the hyaluronidase treatment.
What dangers can hyaluronidase administrations pose?
As per medical research, allergic responses are one issue that might arise after hyaluronidase injection and happen between 0.05% and 0.69% of the time. There seems to be contradictory data on whether hyaluronidase patch testing should really be performed to screen for signs of allergy, with some medical professionals recommending it to reduce the risk of allergic reactions when it is used for elective therapies. I would suggest that the patch testing be performed intradermally and that the physician watches for any itching, irritation, or erythema right after the injection.
"Allergy patch testing"
However, it may be justified to take the hyaluronidase as soon as possible to reduce the danger of future harm if the patient is exhibiting symptoms of vascular occlusion.
I would advise watching the patient for 30 minutes after the hyaluronidase treatment and ensuring they get the proper aftercare instructions. Although I have discovered that for denser, more cross-linked hyaluronic acid, it may take 48 hours for the effects to be visible, results are frequently noticeable immediately. If more hyaluronidase is required, another injection should be administered through follow up session. Read our article "Hyaluronidase And Aesthetic Procedures" for in-depth info.
Conclusion:
Hyaluronidase is a crucial component in the management of HA dermal filler issues, however it shouldn't be used in place of proper technique. Practitioners who believe they are qualified to administer HA fillers and treat patients also need to be able to detect, treat, and manage issues.
The national institute and the US FDA do not have any protocols on the use of hyaluronidase in cosmetic dermatology. It is essential that a protocol be created and put in place so that all injectors can adopt and use to immediately administer hyaluronidase during an emergency scenario, since knowing little about how to use hyaluronidase is insufficient to keep patients safe. A set of guiding principles must be provided by the protocol to aid in decision-making. It doesn't need to be difficult, just clear to all injectors and frequently reviewed. Although it doesn't currently appear to be necessary, patch testing is frequently advised, especially if the situation is not urgent.
Examples of Hyaluronic acid fillers that can be broken down by the hyaluronidase enzyme are: Juvéderm ultra, Juvéderm Voluma, Juvederm Volbella, Juvederm Volux, and Belotero Balance to name a few. Many other related products can also be dissolved by a hyaluronidase treatment as long as it is a hyaluronic acid based dermal filler.
For answering more questions on hyaluronidase administration refer to our article"Hyaluronidase, all questions answered"